Basal Cell Carcinoma
What Is a Basal Cell Carcinoma?
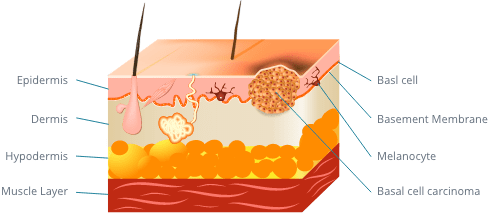
Basal cell carcinomas (BCC) are the most common type of skin cancer, with over 4 million diagnoses occurring every year. These lesions grow from basal cells, which are located in the outer layer of skin, known as the epidermis. When basal cell carcinomas develop, they can take on different forms, often looking like an open sore, shiny bump, red spot, or white patch. Patients with darker skin may have a basal cell carcinoma that looks brown. Although basal cell carcinomas are a very common skin cancer, they are usually curable when treated early and leave minimal damage to the area of the tumor.
- Basal Cell Carcinoma Causes
- Basal Cell Carcinoma Risk Factors
- Signs of Basal Cell Carcinoma
- Where Basal Cell Carcinoma Develops
- Preventing Basal Cell Carcinoma
- Basal Cell Carcinoma Subtypes
- Diagnosing Basal Cell Carcinoma
- Basal Cell Carcinoma Prognosis
- Basal Cell Carcinoma Treatment
- Consequences of Not Treating Basal Cell Carcinoma
What Causes Basal Cell Carcinomas?
Basal cell carcinomas are caused when basal cells in the outer layer of skin are damaged, leading to DNA changes. This most often results from ultraviolet (UV) radiation from the sun or indoor tanning beds, which is the biggest cause of most skin cancers. While UV exposure is the main cause of basal cell carcinomas, a variety of factors contribute to a person’s overall risk of the condition.
Who Is at Risk of Basal Cell Carcinomas?
Knowing whether you are at a higher risk of developing a basal cell carcinoma can help with prevention as well as detecting a lesion in its earlier stages. Risk factors that have been linked to basal cell carcinomas include the following:
- Excess sun exposure or indoor tanning
- History of skin cancer, such as a previous basal cell carcinoma, squamous cell carcinoma or melanoma
- Over the age of 50
- Fair skin
- Male
- Radiation therapy
- Chronic skin infections, injuries, or inflammation
- Predisposing genetic syndromes (ex. Gorlin’s Basal Cell Nevus Syndrome, Rombo Syndrome, Brooke-Spiegler Syndrome, Bazex-Dupré-Christol Syndrome, Schopf-Schulz-Passarge Syndrome, Multiple hereditary infundibulocystic BCC)
While these may indicate someone is at an increased risk of basal cell carcinomas, the disease can still develop in those who do not exhibit these qualities.
What Are the Signs of a Basal Cell Carcinoma?
To identify a basal cell carcinoma or other skin abnormality, you should perform skin exams on yourself regularly, looking for any new or changing lesions. Basal cell carcinomas may become crusty and itchy, as well as bleed or ooze. They can be red, pink, white, translucent, or even pigmented. As a result, this can make it difficult for people to recognize they have the condition. Many people discover they have a basal cell carcinoma because they have a sore that will not seem to heal. This is often a telltale sign of skin cancer.
Where on the Body Do Basal Cell Carcinomas Develop?
Since basal cell carcinomas are often caused by excess sun exposure, they typically manifest in areas of the body that are frequently exposed to the sun. This includes the nose, eyelids, scalp, neck, shoulders, and arms. In fact, over 85% of basal carcinomas have been noted to develop on the head and neck. Basal cell carcinomas most commonly develop in fair-skinned men and women.
How Can I Prevent Basal Cell Carcinomas?
The best ways to prevent basal cell carcinomas is to protect your skin from the sun. Since UV radiation is the most common cause of this type of skin cancer, you can lower your risk of developing the lesions by taking the precautions detailed below:
- Avoid the sun at its peak hours between 10am-4pm
- Refrain from using tanning beds, which still emit harmful UV rays
- Wear sunscreen with an SPF of 30 or higher, even on cloudy days
- Shield your skin with protective clothing and hats
- Wear sunglasses that block UVA and UVB rays
- Do self-skin exams regularly and share any changes with your doctor
- Schedule routine skin exams with your dermatologist
While these steps can help reduce your risk of basal cell carcinomas and other skin cancers, it is still important to regularly check your skin for any abnormal growths. If you have had a basal cell carcinoma removed in the past, recurrence is very common. This is why you should get regular skin exams with your dermatologist at least once per year.
What Are the Different Basal Cell Carcinoma Subtypes?
Basal cell carcinomas come in many forms, which can look and behave differently. If you are diagnosed with a basal cell carcinoma, you may learn you have one of the following subtypes:
- Nodular: The most common type of BCC, making up more than 60% of diagnoses, is the nodular basal cell carcinoma. This presents as a bump that is white or skin-colored, often found on the face. Blood vessels often become more noticeable and can bleed.
- Superficial: Usually appearing on the shoulders and upper trunk areas, a superficial basal cell carcinoma is a slow-growing, invasive subtype that looks like a patch with a rolled border.
- Morpheaform: White or yellow with a waxy appearance, morpheaform (or sclerosing) basal cell carcinomas affect fibroblast growth in the dermis. They develop between collagen fibers and can look like a flat scar. This subtype can be more complicated to diagnose.
- Micronodular: Often found on the back, micronodular basal cell carcinomas can be a raised or yellowish-white flat tumor. They are usually round with a distinct border and develop in a cluster of small nodules.
- Infiltrative: Forming as a thin cluster of whitish lesions, the infiltrative basal cell carcinoma appears in the dermis layer of the face or upper trunk.
- Pigmented: A type of nodular, micronodular, or superficial basal cell carcinoma, the pigmented subtype has more melanin and melanophages, causing it to appear brown or black.
- Basosquamous: Also known as metatypical, the basosquamous carcinoma has features of both BCCs and squamous cell carcinomas. This can be a more aggressive form of skin cancer that grows in an infiltrative pattern.
- Nodulocystic: A variant of the nodular basal cell carcinoma, this type of tumor involves a bluish-gray cyst filled with fluid. Nodulocystic BCCs typically form within the tumor nests.
- Microcystic: Although rare, microcystic basal cell carcinomas can most often be found on the head or neck. They involve cysts filled with keratin, and the cells are located in the bottom layer of the dermis.
- Clear Cell: This is an uncommon type of basal cell carcinoma that is characterized by clear cells, which show deteriorating tumor change.
- Granular Cell: With this subtype, cells have small, pink granules. Similar to clear cell basal cell carcinomas, granular cell BCCs show regressive change in the tumor.
- Signet Ring Cell: Another form of basal cell carcinomas, signet ring cell BCC lesions take on the appearance of a signet ring.
- Solitary: Developing in younger patients, solitary basal cell carcinomas are caused by embryonic fusion clefts in the skin.
- Adenoid: This slow-growing subtype of basal cell carcinomas has a gland-like form with spaces full of mucin. They are often discovered on the scalp.
- Follicular: A variation of basal cell carcinomas, follicular differentiation presents as tumor cells that appear similar to hair follicles. Small infundibular cysts and matrical cells are also found in this subtype.
- Infundibulocystic: Less aggressive compared to other forms, infundibulocystic basal cell carcinoma tumors have follicular and infundibula germs. These cells are typically small and are at a low risk of spreading.
- Neurotropic: These tumors can influence the nervous system and cause pain. Neurotropic basal cell carcinomas are microscopic in size and can be complex to surgically remove.
- Pleomorphic: Appearing on the head or neck, pleomorphic basal cell carcinomas are large, produce mucin, and can have tumors with one or multiple nuclei.
- Rodent Ulcer: When left untreated, a basal cell carcinoma can develop into a rodent ulcer, where the center of the tumor leaves a hole in the skin.
How Is a Basal Cell Carcinoma Diagnosed?
To diagnose a basal cell carcinoma, a biopsy will need to be taken of the lesion. Removing this small section of tissue will allow the cells to be examined under a microscope to detect any abnormal cells. If cancerous basal cells are found, you will be diagnosed with a basal cell carcinoma. The pathology report of your lesion will indicate the type of basal cell carcinoma you have and, in many cases, how deeply the cancerous cells have grown. Based on this information, our board-certified dermatologist, Dr. Adam Mamelak, will recommend the most appropriate form of treatment for your unique case.
What Can I Expect with My Basal Cell Carcinoma Prognosis?
A basal cell carcinoma typically progresses very slowly, making it a very treatable form of skin cancer. When left untreated, however, these cells can grow wide and deep into the skin, invading local tissues, breaking down the skin causing open sores that are prone to infection. Ultimately, basal cell carcinoma can severely disfigure the affected area. Although basal cell carcinomas do not usually spread to other areas of the body, there are rare aggressive cases that can. Treating basal cell carcinomas as soon as possible after diagnosis is important, as the more advanced the tumor is, the more likely it will recur in the future.
What Is the Best Treatment for Basal Cell Carcinoma?
As with any skin cancer, the best treatment for a patient’s basal cell carcinoma will depend on the severity of the disease. Dr. Mamelak may recommend either a topical, oral, or surgical treatment based on the details of your condition.
Topical Treatments
Patients with basal cell carcinoma in its earliest stages are often candidates for non-invasive treatment with topical ointments. The most common prescriptions include 5-Fluorouracil (like Efudex and Carac) and imiquimod, which can help cause regression of the cancerous cells with minimal side effects.
Oral Treatments
Those with aggressive forms of basal cell carcinoma may be recommended treatment with oral medications like Erivedge® or Odomzo®. These are typically only prescribed if the patient is not eligible for surgery or radiation therapy, due to being immunosuppressed or having overly large tumors.
Surgical Treatments
Surgery can be extremely effective for those with mild, moderate, or severe basal cell carcinomas. Potential techniques Dr. Mamelak may perform include:
Cryosurgery
An extremely cold substance, such as liquid nitrogen, is used to freeze the lesion and destroy the cancerous cells. This may be used on small and thin basal cell carcinomas.
Curettage
The skin cells or tumor are excised using a curette, which is a tool with a ring-shaped tip to scrape the area.
Electrodesiccation
Usually performed along with curettage, electrical heat is used to destroy and remove the basal cell carcinoma.
Surgical Excision
The tumor will be surgically removed with a margin of the surrounding skin. This ensures any cancerous cells that have extended beyond the tumor are removed, as well.
Mohs Micrographic Surgery
Mohs surgery has a 99% cure rate and involves the use of a microscope to map the course of the cancer and its roots to achieve complete removal with minimal damage to nearby tissue. This technique is often used for more complex cases of basal cell carcinomas.
Dr. Mamelak always prioritizes the most conservative treatment options that can achieve optimal results. He will listen to your account of your basal cell carcinoma and examine the tumor, recommending the most effective solution for achieving long-term remission.
What Happens if I Don’t Treat a Basal Cell Carcinoma?
Basal cell carcinoma treatments have an extremely high success rate, especially when the lesions are caught early. While basal cell carcinomas rarely spread to other body areas, the tumors can grow in size if not addressed. This can disfigure the area, impact function and movement, and leave significant scars. Although this type of skin cancer is very rarely life-threatening, treating basal cell carcinomas early allows for more conservative treatments to be performed. This can produce better outcomes, ensure more efficient treatments, and reduce the cost of overall treatment.
If you think you may have a basal cell carcinoma, please contact Dr. Mamelak to schedule a skin evaluation.