Melanoma
What Is Melanoma?
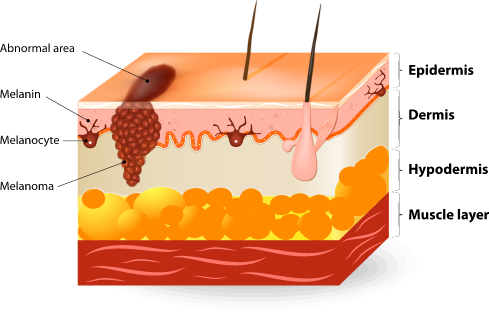
Melanoma is a dangerous form of skin cancer that develops in melanocytes, which are cells found in the outer layer of skin. Although less common than basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), melanoma has become more prevalent and is considered more serious due to its ability to aggressively spread if not treated early. When caught in its beginning stages, nearly 100% of melanoma cases can be cured.
What Causes Melanoma?
The most common cause of melanoma is ultraviolet (UV) radiation from excessive sun exposure. As UV rays damage the skin, this stimulates the production of more melanin, leading to a tan or dark spots. Melanoma develops when UV radiation causes DNA damage, which ultimately leads to changes in the melanocytes. As a result, these skin cells begin to mutate, grow, and become cancerous.
What Are the Symptoms of Melanoma?
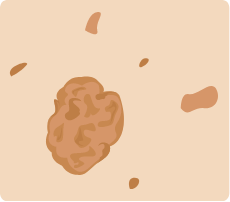
Melanoma usually occurs in moles or normal skin. It can be asymptomatic — without any pain or discomfort — or may offer subtle signs, such as bleeding, changes in color, or a sore that will not heal. If you have any moles or growths, our board-certified dermatologist, Dr. Adam Mamelak, advises you to check them regularly to see if they show changes like asymmetry, irregular border, multiple colors, or increased size.
While melanoma can develop on any skin area, it is most common on the trunk or back for Caucasian men, chest and legs for Caucasian women, and feet and hands for those of Asian, Hispanic, or African descent. In rare cases, melanoma can form around the mouth or eyes. Even more rare, melanoma may present in the genital area, gastrointestinal tract (GI), or genitourinary tract (GU).
What Are the Different Types of Melanoma?
There are four main subtypes of melanoma: superficial spreading, lentigo maligna, nodular maligna, and acral lentiginous. The location of the lesion and appearance of the area will help with your diagnosis and determining the most effective treatment method.

Superficial spreading
Lentigo maligna

Nodular maligna

Acral lentiginous
Am I at Risk of Getting Melanoma?
Although some people are more susceptible to melanoma, this type of skin cancer can affect anyone despite their race or ethnicity. Certain factors increase the risk of getting melanoma, including those with a family history of melanoma. In addition, people with one or more of the following should be especially aware of any changes in their skin:
- Fair skin, blue or light-colored eyes, blonde or red hair
- Living in an area of high altitude or in a sunny region
- Work or participate in activities regularly spent outside
- History of getting blisters from sunburns as a child
- Frequently tan outside or in tanning beds
- Have atypical or dysplastic moles or multiple birthmarks
How Is Melanoma Diagnosed?
If your dermatologist believes a mole or skin lesion is atypical, they may perform a biopsy. This involves taking a small sample of the area, which is then processed in a lab and examined under a microscope. In some cases, a procedure known as a sentinel lymph node biopsy (SLNB) may be recommended, which evaluates if the cancerous cells have spread to your lymph nodes. Other imaging tests, such as X-rays or CT scans, may also be performed to check if the malignant melanoma has spread to other body areas.
What Are My Melanoma Treatment Options?
If you are diagnosed with melanoma, you will need surgery to completely remove the cancerous cells. This will also involve excision of some of the surrounding skin and tissue, depending on how deep your skin cancer has spread, to ensure clear margins. Early stages of melanoma (in situ or stage I) is confined to the outermost layers of skin and can be treated with excision alone, such as through Mohs micrographic surgery. For intermediate melanoma (stage II), an SLNB is needed to check if the cancer has spread to the lymph nodes, which may need to be surgically removed in addition to other possible treatments.
Advanced melanomas (stages III and IV) are considered metastatic, spreading to other areas of the body and other organs. These stages are more difficult to treat and may require additional intervention, such as:
- Chemotherapy to destroy the cancer cells
- Immunotherapy to help the immune system fight the cancer
- Radiation to manage discomfort caused by the spreading of the cancer
- Surgery to alleviate any pain associated with the cancer
In addition to these treatment methods, clinical trials are often available for those who do not respond to traditional melanoma therapies. Dr. Mamelak can discuss this route with you, should you need alternative solutions for treating your skin cancer.
For those who have previously had melanoma removed and recovered, it is essential to regularly examine your skin for any changes or abnormal lesions. Once you are diagnosed with melanoma, you are at a higher risk of developing the cancer again in the future.